Estimated reading time: 17 minutes
Personal care assistance is one of the most delicate acts in home care support. Much more than a simple hygiene gesture, it touches upon the deepest intimacy of the person, their dignity and the image they have of themselves. For home care professionals as well as family caregivers, knowing how to accompany this moment with respect, kindness and professionalism is fundamental.
This comprehensive guide explores all dimensions of respectful personal care: the ethical principles that should guide it, practical techniques to preserve intimacy, the importance of consent, adaptation to individual rhythms and specificities related to certain pathologies. Whether you are starting out in the profession or wish to perfect your practices, this article will guide you toward more humane and more respectful personal care.
The Stakes of Personal Care
A Meaningful Act
Personal care assistance is never a trivial act. For the person receiving it, it often represents:
A confrontation with loss of autonomy: needing help for gestures once performed without thinking can be experienced as an ordeal, a confirmation of decline. This awareness can generate sadness, anger or denial.
An intrusion on intimacy: exposing one’s naked body to a third person, even a professional, disrupts usual social codes. The intimate body, which one generally only shows to closest loved ones, suddenly becomes visible to others.
A reminder of vulnerability: in this situation of dependence, the person may feel fragile, exposed, at the mercy of another. This vulnerability can reactivate difficult memories or generate anxiety.
But also a moment of care and relationship: when well accompanied, personal care can become a privileged time of well-being, communication and human connection.
Fundamental Rights at Stake
Personal care involves several fundamental rights of the person:
The right to dignity is at the heart of this act. Human dignity is inalienable: it is not diminished by illness, disability or dependence. Personal care must be performed in a way that preserves and affirms this dignity.
The right to privacy implies that intimate parts of the body are only exposed when strictly necessary, that the door is closed, that windows are covered, that personal care is not performed in front of third parties.
The right to consent means that the person must be informed, as much as possible, of the acts that will be performed and that they must be able to accept or refuse them.
The right to respect for habits and preferences recognizes that each person has their own rituals, preferences, relationship with their body and hygiene, which must be respected as much as possible.
Preparing for the Personal Care Moment
The Environment: Creating a Secure Space
Preparation of the environment largely conditions the experience of personal care:
Room temperature should be sufficiently high (at least 72-75°F) to prevent the person from being cold once undressed. Preheat the bathroom if necessary.
Lighting must be sufficient to work safely but not harsh. Avoid harsh fluorescent lights that harden features and prefer soft lighting.
Privacy must be guaranteed: close the door, draw curtains or blinds if the window faces outside.
Equipment must be prepared in advance and within reach: clean towels, washcloths, soap or shower gel, shampoo if necessary, clean clothes, changes if needed, moisturizer…
Safety must be ensured: non-slip mat in the bathtub or shower, grab bars if necessary, adapted shower seat.
Preliminary Communication: Informing and Reassuring
Before starting, take time to talk with the person:
Announce what you will do: “It’s time for personal care, we’re going to the bathroom together.” This announcement allows the person to prepare mentally.
Propose rather than impose: “Do you prefer to start with your face or your feet?”, “Do you want to use a washcloth or the sponge?” These small choices give back control to the person.
Be attentive to their current state: fatigue, pain, anxiety can influence how personal care unfolds. If the person is not well, adapt accordingly.
Respect refusals as much as possible. If the person categorically refuses, don’t insist forcefully. Try to understand the reason for refusal, offer to postpone, or to do things differently.
Consent: A Non-Negotiable Pillar
What Is Consent in Personal Care?
Consent is the agreement given by a person for an act concerning them to be performed. In personal care, it implies:
- That the person is informed of what will be done
- That they understand this information
- That they are free to accept or refuse
- That they can withdraw consent at any time
Consent is not obtained once and for all: it must be renewed at each personal care session, as the person’s state and wishes may vary.
Seeking Consent Despite Cognitive Disorders
When the person has cognitive disorders, the question of consent becomes more complex. This does not mean it should be abandoned, quite the contrary: even a severely affected person retains a capacity for feeling and expression that must be decoded.
Adapt your communication: short and simple sentences, warm tone, kind gaze, gentle and predictable gestures.
Observe non-verbal signals: tension, grimacing, pulling back indicate discomfort or refusal. Relaxation, a smile, cooperation signal acceptance.
Proceed in steps: announce each gesture before performing it, wait for a sign of acceptance (even minimal) before continuing.
Respect even non-verbal refusals: if the person stiffens, closes their eyes, turns their head away, struggles, it is a refusal that must be heard.
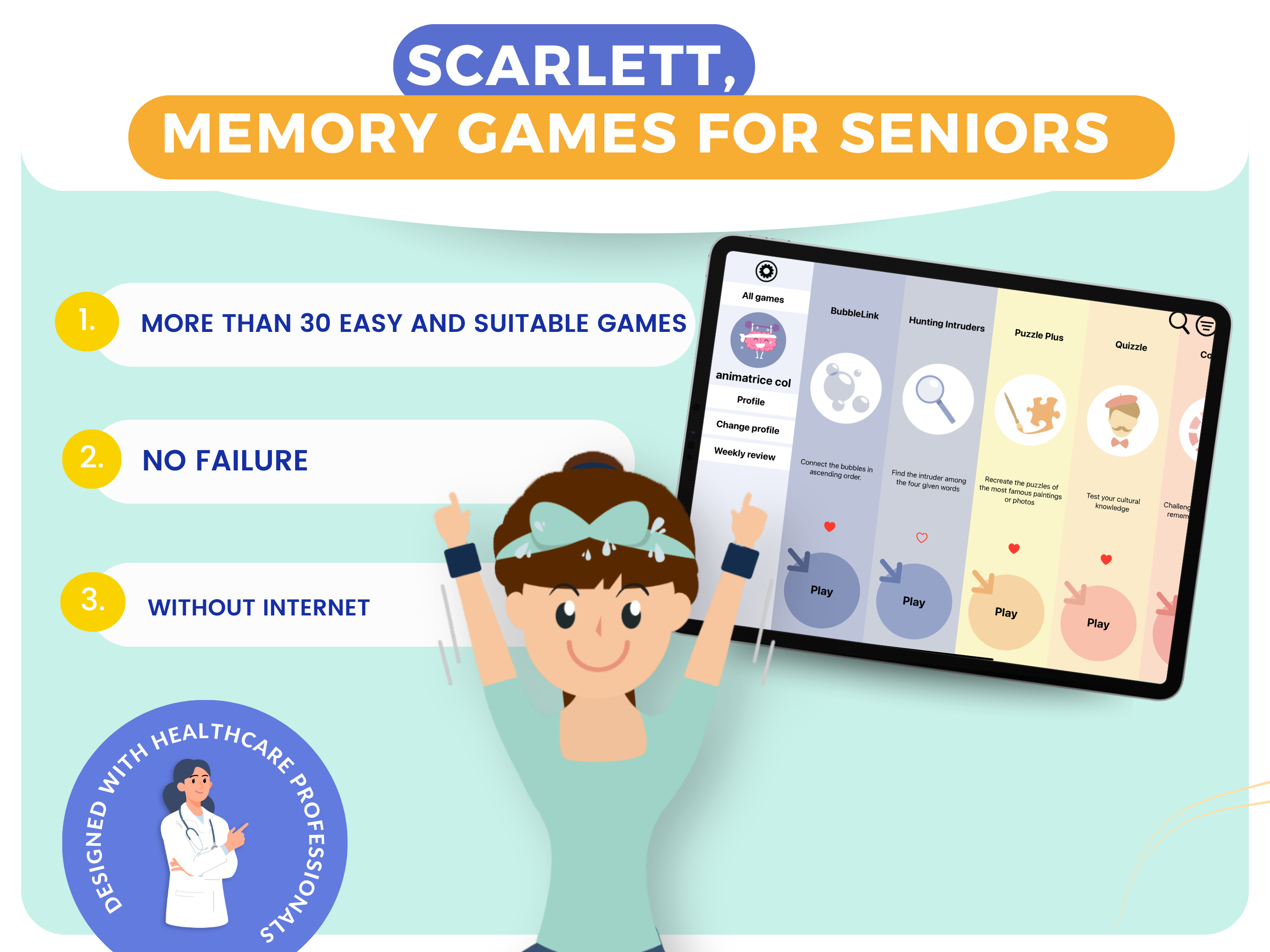
DYNSEO’s SCARLETT program can contribute to maintaining communication and comprehension abilities in people with cognitive disorders. By regularly stimulating cognitive functions, SCARLETT helps people stay “present” longer and capable of expressing their preferences, including during intimate care moments like personal care.
Facing Refusal: Understanding Before Acting
Refusal of personal care is common, especially among elderly people or those with cognitive disorders. Before trying to work around it, it is essential to understand the possible reasons:
Modesty and embarrassment: the person may be embarrassed to expose their body, especially if the caregiver is of the opposite sex or if it’s a new face.
Fear: fear of water, cold, slipping, pain related to movements.
Misunderstanding: the person may not understand what is being asked of them or why.
Traumatic memories: personal care can reactivate painful memories (past abuse, difficult medical experiences…).
Opposition as self-affirmation: for a person who feels they are subjected to everything, saying no may be the last way to exercise control.
Physical discomfort: pain, fatigue, malaise can make personal care unbearable.
Facing refusal, the right approach is to:
- Not force physically
- Not make the person feel guilty
- Try to understand the reason for refusal
- Offer alternatives (partial care, postponement, different caregiver…)
- If refusal persists and hygiene becomes a health problem, alert the supervisor and care team to find an appropriate solution
Preserving Intimacy: Gestures That Make the Difference
The Minimal Uncovering Technique
The principle is simple: only uncover the part of the body being washed, other parts remaining covered. This technique respects modesty and limits the feeling of cold.
In practice:
- The person remains covered with a towel or bathrobe
- Only the area to be washed is uncovered, washed, dried, then recovered
- Move to the next area by uncovering progressively
- Intimate parts are uncovered as briefly as possible
Bed Bath: Preserving Dignity
When the person cannot get up, bed bathing requires particular attention to privacy:
- Close the bedroom door
- Place a screen if other people may enter
- Use a sheet or bath towel to cover the person
- Proceed by area keeping the rest of the body covered
- Change water regularly
- Make sure the person is not cold
The Gaze: A Key Element
Your gaze says a lot about the respect you have for the person:
- Avoid staring at the person’s intimate parts
- Look the person in the eyes when speaking to them
- Keep a neutral and kind gaze, without disgust or excessive embarrassment
- If you need to look at an intimate area to perform care, announce it and remain professional
Words: Choosing Carefully
Words used during personal care contribute to creating a respectful climate or, conversely, a humiliating one:
To absolutely avoid:
- Infantilizing terms: “we’re going to go potty”, “you’re all dirty”
- Comments about the body: “you’ve lost weight”, “it’s dirty”
- Judgments: “you stink”, “you soiled yourself again”
- Abrupt formal address for a person used to informal address, or vice versa
- Talking about the person in third person in their presence
To favor:
- A calm and warm tone
- Respectful formulations: “I’m going to help you freshen up”
- Positive encouragement: “there, that’s good”
- Naming body parts in a neutral and adult way
- Systematic announcement of what you will do
Respecting Individual Rhythms
Understanding Elderly People’s Relationship with Time
Elderly people, particularly those with cognitive disorders, have a different relationship with time than ours. They need more time to:
- Understand what is being asked of them
- Make decisions
- Perform movements
- Adapt to changes
This slower tempo is not ill will: it corresponds to neurological and physiological changes related to age.
Adapting Your Pace
Personal care should not be a race against time. Certainly, professionals have time constraints, but:
Take time to create the relationship: a few minutes of exchange before starting allow the person to prepare and relax.
Let the person do what they can: even if it’s slower, encourage them to perform gestures they are capable of. This active participation preserves self-esteem and maintains abilities.
Respect the person’s rhythm: don’t rush them, don’t pull on their limbs, don’t go faster than they can follow.
Plan breaks if personal care is tiring for the person: they can sit for a few moments, catch their breath.
Habits: An Essential Reference Point
Each person has their personal care rituals, built over a lifetime:
Schedules: some prefer personal care in the morning upon waking, others in the evening, still others at another time.
Order of gestures: starting from top or bottom, face first or last…
Products used: particular soap, cologne, specific cream…
Duration and intensity: quick shower or prolonged bath, vigorous or gentle washing…
Take time to learn these habits and respect them as much as possible. They are reassuring reference points for the person and maintaining them contributes to their well-being.
Specificities According to Situations
Personal Care for People with Cognitive Disorders
Personal care for people with Alzheimer’s’s disease or related diseases requires specific adaptations:
Simplify as much as possible: a streamlined environment, simple instructions, a ritualized process.
Stay in the field of vision: always approach from the front, never surprise the person with a gesture coming from behind.
Guide rather than do instead: accompany the person’s gesture rather than doing it for them. “We take the washcloth… we wet it… we wash the face…”
Use procedural memory: automatic gestures are often preserved longer than memory of facts. Placing the washcloth in the person’s hand may be enough to trigger the washing gesture.
Manage behavioral disorders: refusal, agitation, aggression may occur. Stay calm, speak softly, try to understand what is disturbing, offer to take a break or postpone.
Personal Care for People at End of Life
At end of life, personal care takes on a particular dimension:
Adapt the intensity: personal care can be simplified, focused on comfort rather than complete hygiene.
Be particularly gentle: skin becomes fragile, pain is frequent, the slightest movement can be uncomfortable.
Prioritize sensory well-being: lukewarm water, slow gestures, light fragrance if the person appreciates it, moisturizer application.
Absolutely respect refusals: if the person no longer wants complete personal care, it is their most absolute right.
Involve family if they wish: some loved ones wish to participate in this intimate end-of-life moment.
Personal Care for People with Pain
When the person suffers from chronic pain (osteoarthritis, bedsores, wounds…):
Assess pain before starting: if pain is too intense, postpone or adapt personal care.
Coordinate with the care team: personal care can be scheduled after taking pain medication to benefit from its maximum effect.
Mobilize with caution: avoid abrupt movements, support painful limbs, use adapted equipment (patient lift, transfer board…).
Adapt the technique: bed bath rather than shower if transfers are too painful, washcloth bath rather than full shower…
Hygiene Care: Best Practices
Face Care
The face is the most identity-defining part of the body. Take care of it with attention:
- Start with the face, on clean and rested skin
- Use lukewarm water and a gentle product
- Clean eyes from inside to outside, with a different compress for each eye
- Don’t forget the ears (auricle and back of ear)
- Offer shaving for men, facial hair removal if the woman was used to it
- Apply moisturizer if skin is dry
Body Care
Upper body: armpits, chest, back, arms. Focus on armpits, perspiration area. Dry folds well to avoid fungal infections.
Abdomen: clean gently, particularly the navel which can accumulate deposits.
Lower body: legs, feet. Pay particular attention to spaces between toes, drying thoroughly to prevent fungal infections.
Intimate Care
This is the most delicate moment of personal care:
- Always announce what you will do
- Proceed with gentleness and speed, without rushing
- For women: from front to back to avoid urinary infections
- For men: gently retract foreskin to clean glans, then replace
- Rinse thoroughly and dry folds well
- When changing: clean thoroughly after each change to prevent irritation
Shampooing
Hair washing can be performed:
- In the shower if the person can tolerate it
- At the sink with a shampoo basin
- In bed with an inflatable basin and drainage system
Use gentle shampoo, massage scalp delicately, rinse abundantly and dry thoroughly.
Foot and Nail Care
Feet are often neglected when they require particular attention:
- Wash between toes and dry thoroughly
- Observe skin condition (cracks, fungal infections, corns…)
- Apply moisturizer if necessary
- Nail trimming should be performed by a podiatrist for diabetic people or those with circulatory disorders
After Personal Care: Finalizing with Respect
Dressing
Dressing is an integral part of the personal care moment:
- Offer the person to choose their clothes if possible
- Respect their usual clothing style
- Adapt clothing to autonomy (adapted closures, comfortable materials…)
- Help without doing instead: guide gestures, let the person participate
Finishing Touches
These small gestures greatly contribute to well-being:
- Hair styling: respect the person’s usual hairstyle
- Perfume or cologne: use the person’s usual products
- Makeup if the person was used to wearing makeup
- Jewelry if they usually wore it
Comfortable Installation
After personal care, ensure the person is comfortably settled:
- Adapted position (in chair, in bed…)
- Within reach: remote control, call bell, glass of water…
- Room at good temperature
Training: Continuous Improvement
The Importance of Initial and Continuing Training
Personal care is learned and perfected throughout one’s career. Quality training allows one to:
- Master technical gestures safely
- Understand ethical issues of intimate care
- Know how to adapt intervention to different pathologies
- Develop relational skills
- Prevent professional burnout
The training “Stimulate and Create Connection with DYNSEO Games” allows home care professionals to develop their relational skills. While it does not specifically address personal care, it provides essential keys to better communicate with accompanied persons, particularly those with cognitive disorders. This ability to create connection and communicate in an adapted way is fundamental to succeed in delicate moments like personal care.
Resources for Progress
The Home Care Toolkit developed by DYNSEO offers practical resources to enrich daily support. It includes advice sheets, stimulation activity ideas and communication tools that can transform personal care moments into true quality relational time.
Taking Care of Yourself to Take Care of Others
The Emotional Burden of Intimate Care
Accompanying people in their intimacy is not trivial for the caregiver either:
- Daily confrontation with aging, sick bodies, sometimes at end of life
- Exposure to others’ nudity
- Managing refusals, sometimes aggression
- Weight of responsibility
- Repetitiveness of gestures
This emotional burden can lead to burnout if not recognized and addressed.
Preservation Strategies
To last in this profession while remaining kind and professional:
Talk about what you experience: with your colleagues, your supervisor, during team meetings. Putting words to difficult situations helps digest them.
Train regularly: training brings new skills but also perspective and time to exchange with peers.
Take care of your body: personal care gestures are physically demanding. Protect your back, use adapted equipment, don’t hesitate to ask for help in complex situations.
Preserve your personal life: know how to disconnect, recharge, maintain activities and relationships outside of work.
Recognize your value: the home care profession is essential but often little recognized. Be proud of what you bring to the people you support.
Case Studies: Common Situations and Solutions
The Person Who Systematically Refuses Personal Care
Analysis: identify possible reasons (modesty, fear, misunderstanding, opposition, discomfort…).
Solutions to try:
- Change caregiver (male/female, new person/known person)
- Offer another time of day
- Start with less intrusive partial care
- Offer an alternative: refreshing wipes if shower is refused
- Work on the relationship outside of personal care moments
- If refusal persists and poses a health problem, solicit the care team and possibly a geriatrician or psychiatrist
The Person Who Has Inappropriate Behaviors
Analysis: behaviors with sexual connotations may occur, related to disinhibition caused by certain pathologies or confusion between personal care and couple intimacy.
Course of action:
- Keep your calm and professionalism
- Refocus firmly but without aggression: “No, that’s not possible, I’m here to help you wash”
- Cover the person and take a break if necessary
- Systematically report these behaviors to your supervisor
- Don’t blame yourself: you are in no way responsible for these behaviors
- Request a caregiver change if necessary
The Person Who Cries During Personal Care
Analysis: tears can express sadness about loss of autonomy, shame, memory of difficult moments, or simply the need to be heard.
Course of action:
- Stop what you’re doing and pay attention to the person
- Offer them to talk if they wish
- Validate their emotion: “I understand this is difficult”
- Offer to take a break or postpone personal care
- Report these episodes to the team to adapt support
Conclusion: Making Personal Care a Moment of Dignity
Personal care, when performed with respect, attention and professionalism, can become much more than a simple hygiene act. It can be a moment of physical and psychological well-being, authentic human relationship, recognition of the person’s dignity.
The keys to respectful personal care are:
- Systematic seeking of consent, even in cases of cognitive disorders
- Preservation of privacy at every moment
- Respect for the person’s rhythms and habits
- Adaptation to specificities of each situation
- Kindness in gestures, gazes and words
- Training and continuous improvement of practices
Each personal care session is an opportunity to reaffirm the dignity of the person you support. Through your professional gestures and respectful attitude, you tell them: “You are a person worthy of respect and attention, despite illness, despite dependence.”
DYNSEO is committed alongside home care professionals to accompany them in this essential mission. The SCARLETT program contributes to maintaining cognitive abilities, the “Stimulate and Create Connection” training strengthens relational skills, and the toolkit offers concrete resources for quality support.
Together, let’s make every moment of care a moment of dignity.
—
Additional DYNSEO Resources:
—
Article written by DYNSEO, specialist in digital solutions for healthy aging and support for cognitive disorders.






