Stroke, a debilitating cerebrovascular event, strikes with suddenness and severity, altering lives in an instant. Defined as the disruption of blood flow to the brain, strokes manifest in various forms, from ischemic to hemorrhagic, each demanding immediate attention and innovative intervention. The significance of pioneering stroke treatments cannot be overstated; they hold the promise of mitigating long-term disabilities and saving countless lives.
In medical research and practice, the quest for novel stroke therapies stands as a beacon of hope, driving experts to explore uncharted territories and push the boundaries of conventional treatment modalities. This paper explores the dynamic realm of stroke treatment innovation, bridging the gap between research endeavors and clinical application. By elucidating the definition of stroke, underscoring the imperative of innovative interventions, and outlining the purpose of this discourse, we embark on a journey toward understanding and embracing the transformative potential of cutting-edge stroke therapies.
Understanding Stroke
Stroke, a multifaceted cerebrovascular event, encompasses various types, including ischemic strokes resulting from blocked arteries and hemorrhagic strokes caused by ruptured blood vessels. These distinct categories arise from diverse causes and risk factors, ranging from hypertension and diabetes to smoking and sedentary lifestyles. The repercussions of stroke reverberate beyond individual patients, exerting profound impacts on families, communities, and society at large. Patients grappling with stroke often confront debilitating physical impairments, cognitive deficits, and emotional challenges, while caregivers shoulder immense burdens of care and support. Societal ramifications encompass economic strains, healthcare resource allocation, and public health initiatives aimed at prevention and rehabilitation. Understanding the nuanced landscape of stroke, encompassing its types, causative factors, and societal implications, is imperative for fostering comprehensive approaches to prevention, treatment, and support.
Traditional Stroke Treatments
Traditional stroke treatments encompass a triad of pharmacological interventions, surgical procedures, and rehabilitation therapies aimed at mitigating the devastating effects of cerebrovascular events. Pharmacological interventions often include thrombolytic agents such as tissue plasminogen activator (tPA) administered to dissolve blood clots in ischemic strokes, along with medications to manage risk factors like hypertension and hyperlipidemia. Surgical procedures encompass a spectrum of interventions ranging from carotid endarterectomy to remove plaque buildup in arteries to endovascular procedures like mechanical thrombectomy for clot removal. Rehabilitation therapies form a cornerstone of stroke recovery, encompassing physical, occupational, and speech therapy modalities tailored to restore motor function, enhance cognitive abilities, and improve communication skills. Despite advancements in stroke treatment, traditional approaches underscore the importance of multidisciplinary interventions spanning acute care to long-term rehabilitation in optimizing patient outcomes and fostering recovery.
Evolution of Stroke Treatment
The evolution of stroke treatment represents a journey of remarkable progress and innovation, characterized by leaps in understanding, technology, and patient care. This journey has transformed the prognosis for stroke survivors, turning what was once considered an insurmountable challenge into a condition that can be effectively managed and, in many instances, significantly rehabilitated. The introduction of groundbreaking technologies, sophisticated imaging techniques, and cutting-edge therapies has revolutionized the way strokes are treated, offering new hope and possibilities for recovery.
Telestroke and Remote Assessments: The advent of telestroke systems has been a game-changer in extending the reach of stroke specialists across the globe. This technology allows for immediate remote assessment and treatment decision-making, connecting patients in rural or underserved areas with stroke experts within minutes. Such rapid consultation ensures that critical time windows for treatment are not missed, significantly improving outcomes. This democratization of access to specialized care is a testament to the transformative power of technology in healthcare.
Advanced Imaging Techniques: The strides made in imaging technology have provided clinicians with a window into the brain’s intricate workings, offering detailed views that were previously unattainable. MRI and CT scans can now reveal the extent and location of a stroke with precision, enabling tailored treatment plans that address the specific needs of each patient. These imaging advancements not only facilitate accurate diagnoses but also help in monitoring the progress of recovery, guiding rehabilitation efforts in a more informed and effective manner.
Targeted Therapies and Personalized Medicine: Perhaps one of the most exciting developments in stroke treatment has been the shift towards personalized medicine. Targeted therapies, such as neuroprotective agents designed to shield the brain from further damage, and endovascular devices that can remove or dissolve clots, reflect a move towards treatments that cater to the individual circumstances of each stroke. This approach not only improves the chances of a successful outcome but also minimizes the risk of adverse effects, marking a significant step forward in patient care.
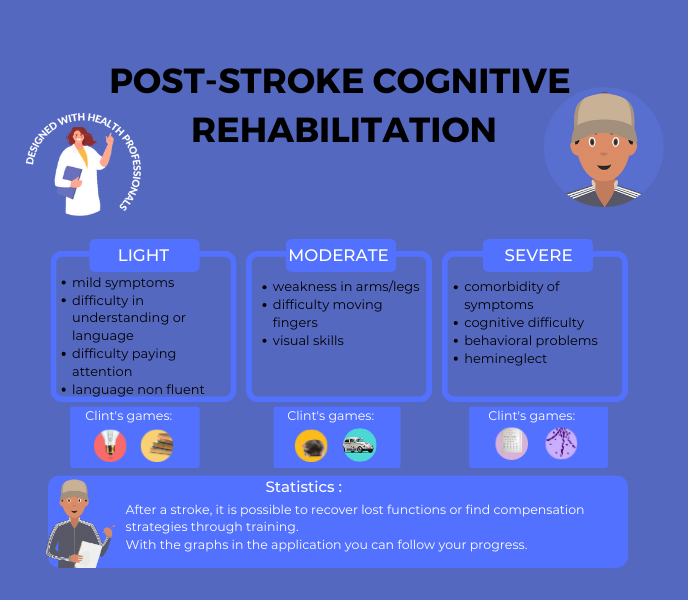
The Role of Brain Training Technologies: In this evolving landscape, innovative solutions like brain training platforms, such as our client Brain Training, are emerging as vital tools in post-stroke rehabilitation. These platforms offer exercises designed to improve cognitive functions such as language, memory, and problem-solving skills, which are often affected by stroke. By leveraging the principles of neuroplasticity—the brain’s ability to reorganize itself by forming new neural connections—brain training can significantly enhance recovery and quality of life for stroke survivors. Such technologies embody the future of stroke rehabilitation, where digital tools and personalized therapy plans converge to support the brain’s healing process.
As we look to the future, the evolution of stroke treatment continues to be driven by innovation, research, and a deepening understanding of the brain’s resilience. The integration of telemedicine, advanced imaging, targeted therapies, and rehabilitation technologies like Brain Training illustrates a comprehensive approach to stroke care that is not only more effective but also more compassionate. This holistic view of treatment and recovery points to a future where the impact of stroke is significantly diminished, and survivors have access to the best possible outcomes.
Research Initiatives in Stroke Treatment
Research initiatives in stroke treatment have ushered in a new era of therapeutic possibilities, with a focus on stem cell therapy, gene therapy, and neuroprotective strategies. Stem cell therapy holds promise in harnessing the regenerative potential of various stem cell types to repair damaged brain tissue, promote neurogenesis, and enhance functional recovery post-stroke. Gene therapy explores the genetic underpinnings of stroke susceptibility and recovery, aiming to modulate gene expression to attenuate neuronal damage, promote neuroplasticity, and mitigate long-term sequelae. Additionally, neuroprotective strategies encompass a diverse array of interventions aimed at preserving neuronal integrity, reducing oxidative stress, and mitigating inflammatory responses following stroke onset. These research endeavors represent pioneering approaches to stroke treatment, offering tantalizing prospects for enhancing therapeutic efficacy and improving patient outcomes in the quest to combat one of the leading causes of morbidity and mortality worldwide.
Translating Research into Practice
Translating research into practice in the realm of stroke treatment requires navigating a complex landscape marked by clinical trials, evidence-based medicine, regulatory approvals, and implementation challenges. Clinical trials serve as the cornerstone of evidence-based medicine, validating the safety and efficacy of novel interventions before they can be adopted into clinical practice. Regulatory approvals and guidelines set forth by governing bodies such as the FDA ensure that emerging treatments meet rigorous standards of safety and efficacy, safeguarding patient welfare. However, the translation of research findings into routine clinical care is not without its hurdles. Implementation challenges, including resource constraints, technological barriers, and clinician training requirements, pose formidable obstacles to the widespread adoption of innovative stroke treatments. Overcoming these challenges demands concerted efforts from stakeholders across the healthcare continuum to bridge the gap between research discoveries and real-world patient care, ultimately improving outcomes and quality of life for individuals affected by stroke.
Promising Innovations in Stroke Treatment
Telemedicine and Remote Monitoring
Robotics and Rehabilitation
The integration of robotics into stroke rehabilitation programs holds immense promise for enhancing motor recovery, functional independence, and quality of life among stroke survivors. Robotic devices offer precise, repetitive, and customizable therapy modalities tailored to individual patient needs, enabling intensive and targeted rehabilitation interventions. These technologies facilitate task-specific training, proprioceptive feedback, and adaptive assistance, promoting neural plasticity and motor learning in the damaged brain. By augmenting traditional rehabilitation approaches, robotics empower patients to achieve meaningful gains in mobility, dexterity, and activities of daily living, thereby facilitating reintegration into society and optimizing long-term functional outcomes post-stroke. As robotics continue to evolve, they represent a pivotal tool in the rehabilitation arsenal, offering new avenues for restoring lost function and maximizing recovery potential in stroke survivors.
Artificial Intelligence in Stroke Management
Artificial intelligence (AI) is poised to revolutionize stroke management by offering novel insights into disease pathophysiology, optimizing treatment decision-making, and improving prognostication accuracy. AI algorithms analyze vast amounts of clinical data, imaging studies, and biomarkers to identify patterns, predict outcomes, and tailor treatment strategies to individual patient profiles. Machine learning models aid in early stroke detection, triage, and risk stratification, enabling healthcare providers to prioritize interventions and allocate resources effectively. Moreover, AI-driven imaging analysis enhances diagnostic accuracy, facilitates lesion segmentation, and guides treatment selection, thereby expediting time-sensitive interventions such as thrombolysis and endovascular therapy. By harnessing the power of artificial intelligence, stroke management is poised to enter a new era of precision medicine, where interventions are personalized, outcomes are optimized, and lives are saved.
Collaborative Approaches in Stroke Care
Collaborative approaches in stroke care are pivotal in addressing the multifaceted needs of patients and optimizing outcomes through synergistic efforts. Multidisciplinary teams and comprehensive care models bring together specialists from diverse disciplines including neurology, rehabilitation, nursing, and social work to provide holistic and patient-centered care. By fostering interdisciplinary communication and coordination, these teams streamline care delivery, minimize treatment gaps, and optimize resource utilization, ultimately enhancing the quality and continuity of care across the stroke care continuum. Public-private partnerships play a crucial role in bridging funding gaps, facilitating technology transfer, and driving innovation in stroke research, treatment, and prevention initiatives. Additionally, international collaboration and knowledge-sharing initiatives foster the exchange of best practices, research findings, and clinical insights, facilitating cross-cultural learning, benchmarking, and capacity building in stroke care delivery worldwide. Through collaborative endeavors, stakeholders can leverage collective expertise and resources to address the complex challenges posed by stroke, ultimately improving outcomes and quality of life for individuals affected by this debilitating condition.
Addressing Equity and Access to Innovative Treatments
Addressing equity and access to innovative treatments in stroke care necessitates confronting socioeconomic barriers and disparities that disproportionately affect vulnerable populations. Socioeconomic factors such as income level, education, and geographic location often serve as barriers to accessing timely and high-quality stroke care, exacerbating disparities in outcomes and exacerbating health inequities. Strategies for ensuring inclusivity and accessibility encompass implementing community-based outreach programs, enhancing health literacy, and promoting culturally competent care delivery models tailored to the unique needs of diverse populations. Additionally, policy implications and advocacy efforts play a pivotal role in advocating for healthcare policies that prioritize equity, expand access to innovative treatments, and allocate resources equitably across underserved communities. By addressing socioeconomic determinants, implementing targeted interventions, and advocating for policy reforms, stakeholders can strive towards achieving health equity and ensuring that all individuals, regardless of socioeconomic status, have equitable access to life-saving stroke treatments and interventions.
Challenges and Opportunities in the Field
In the dynamic field of stroke treatment, challenges and opportunities abound, shaping the trajectory of care delivery and innovation. Cost-effectiveness and sustainability emerge as paramount concerns, as healthcare systems strive to balance the imperative of delivering high-quality care with fiscal responsibility. Ethical considerations and patient consent loom large in the era of advanced interventions, prompting critical reflections on autonomy, beneficence, and justice in the context of stroke treatment decision-making. Amidst these challenges, future trends and potential breakthroughs offer glimmers of hope, fueled by advancements in precision medicine, telehealth, and regenerative therapies. From personalized treatment algorithms to novel neuroprotective agents, the landscape of stroke care is poised for transformative evolution, promising improved outcomes, enhanced patient experiences, and a brighter future for individuals affected by this devastating condition. By navigating challenges, embracing opportunities, and prioritizing innovation, stakeholders can chart a course towards a more equitable, sustainable, and patient-centered approach to stroke treatment and prevention.
This exploration of stroke treatment underscores the critical importance of continued innovation, collaboration, and advocacy in the quest to improve outcomes and enhance the quality of life for individuals affected by stroke worldwide. Key findings reveal the multifaceted nature of stroke care, spanning from traditional treatments to promising innovations such as telemedicine, robotics, and artificial intelligence. As we reflect on the strides made in stroke treatment, it becomes evident that sustained innovation and collaboration are essential for addressing existing challenges and unlocking new frontiers in care delivery. Therefore, a concerted call to action is needed to prioritize stroke care on national and global agendas, advocate for equitable access to treatments, and foster interdisciplinary partnerships aimed at driving meaningful change. By uniting efforts, embracing innovation, and advocating for policy reforms, we can usher in a new era of stroke care characterized by improved outcomes, enhanced quality of life, and greater hope for all those impacted by this debilitating condition.
AND FOR FURTHER INFORMATION

CLINT, YOUR BRAIN COACH
With your JOE brain coach, you choose which cognitive functions to target: attention, concentration, executive functions, mental agility, strategy implementation, etc. A fun, efficient program that supports you every day.
Other articles that might interest you:
Reconstructing After Stroke: Redefining Identity and Goals.
A stroke is a serious medical condition that occurs when blood flow to the brain is interrupted, causing damage to...
The Different Types of Stroke Explained: Ischemic, Hemorrhagic and TIA.
A stroke is a serious medical condition that occurs when blood flow to a part of the brain is interrupted or reduced,...
Preventing Stroke Recurrence: Measures and Lifestyle Changes.
A stroke is a serious medical condition that occurs when blood flow to the brain is interrupted, causing damage to...