Ischemic stroke is the most common type, accounting for around 85% of all strokes. It occurs when the blood supply to the brain is blocked by a blood clot or plaque in an artery. Hemorrhagic stroke occurs when a blood vessel in the brain ruptures, causing a hemorrhage.
Ischemic stroke: causes, symptoms and treatment
The causes of ischemic stroke can vary, but are generally linked to risk factors such as high blood pressure, diabetes, high cholesterol and smoking. Other risk factors include obesity, a sedentary lifestyle and excessive alcohol consumption.
Symptoms of ischemic stroke can vary depending on the part of the brain affected, but can include weakness or paralysis on one side of the body, difficulty speaking or understanding language, vision problems and dizziness.
The aim of ischemic stroke treatment is to restore blood flow to the brain as quickly as possible. This can be done by using thrombolytic drugs to dissolve the blood clot, or by performing surgery to remove the clot. Rehabilitation is also an important part of the treatment, helping patients to recover their motor and cognitive functions.
Hemorrhagic stroke: symptoms, causes and management
Symptoms of hemorrhagic stroke can include sudden, intense headaches, nausea and vomiting, weakness or paralysis on one side of the body, vision problems and convulsions. These symptoms may appear suddenly and require immediate medical attention.
Hemorrhagic stroke can be caused by uncontrolled high blood pressure, vascular malformations, the use of certain anticoagulant drugs or head trauma.
Hemorrhagic stroke management aims to control the hemorrhage and prevent further brain damage. This may require surgery to repair the damaged blood vessel or to evacuate blood accumulated in the brain. Rehabilitation is also essential to help patients recover function and reduce long-term complications.
Risk factors common to both types of stroke
There are several risk factors that can increase the likelihood of having a stroke, whether it’s an ischemic stroke, where the blood supply to part of the brain is blocked, or a hemorrhagic stroke, where a ruptured blood vessel causes bleeding in the brain. These risk factors fall into two main categories: modifiable factors, which we can control and reduce through lifestyle changes or medical treatment, and non-modifiable factors, which are beyond our control.
Modifiable risk factors :
- High blood pressure: The risk of stroke increases with high blood pressure. Effective management of blood pressure through a healthy diet, regular exercise and, if necessary, medication, is crucial.
- Diabetes: Uncontrolled diabetes increases the risk of stroke by affecting the blood vessels. Rigorous blood glucose control is essential.
- Hypercholesterolemia: High levels of bad cholesterol (LDL) can contribute to the build-up of plaque in the arteries, increasing the risk of stroke. A diet low in saturated fats and cholesterol, accompanied by medication where necessary, can help.
- Smoking: Smoking damages blood vessels and can increase the risk of stroke. Quitting smoking is one of the most beneficial changes you can make for your vascular health.
- Obesity: Excess weight increases the risk of stroke. A healthy diet and regular physical activity are essential to achieving and maintaining a healthy weight.
- Sedentary lifestyle: Physical inactivity increases the risk of stroke. Regular exercise, such as brisk walking, swimming or cycling, can reduce this risk.
- Excessive alcohol consumption: Drinking large quantities of alcohol can increase blood pressure and the risk of stroke. It is advisable to limit alcohol consumption.
Non-modifiable risk factors :
-
- Age: The risk of stroke increases with age, particularly after 55. While we can’t stop time, increased awareness and proactive management of other risk factors can help reduce overall risk.
- Gender: Statistically, men are more likely to suffer a stroke at a younger age, but women are more likely to die from it. Gender-specific prevention strategies can be important.
- Family history of stroke: If members of your family have had a stroke, your risk may be higher. While you can’t change your genetics, being aware of this additional risk can encourage you to take the management of modifiable factors seriously.
Stroke in young people: why is it different?
Stroke is not just a condition that affects the elderly. It can also occur in young people, although less frequently. The causes of stroke in young people can be different from those in the elderly.
Common causes of stroke in young people include congenital vascular malformations, blood disorders such as sickle cell anemia, infections, head trauma and illicit drug use. Stroke symptoms in young people can also be different, with severe headaches, impaired vision and seizures being more common.
Stroke treatment for young people is similar to that for older people, but may require a more specific approach depending on the underlying cause of the stroke. Rehabilitation is also important to help young patients regain function and prevent long-term complications.
Stroke in women: specific risk factors

Women may have specific risk factors that increase their risk of stroke. These factors include taking oral contraceptives, pregnancy, menopause and certain medical conditions such as preeclampsia and polycystic ovary syndrome.
Stroke symptoms in women may also differ from those in men. Women are more likely to experience symptoms such as severe headaches, facial pain, pain in the arms and legs, and speech problems.
Stroke treatment for women is similar to that for men, but may require a more specific approach depending on specific risk factors. It’s important for women to be aware of these factors and consult a healthcare professional if they experience stroke symptoms.
Stroke in the elderly: how to prevent and treat it
Older people are more likely to develop stroke due to the accumulation of risk factors over time. Common risk factors in the elderly include high blood pressure, diabetes, high cholesterol, heart disease and a family history of stroke.
Stroke symptoms in the elderly may be similar to those in other age groups, but they can also be more subtle. The elderly may experience symptoms such as confusion, disorientation, general weakness and fatigue.
Stroke treatment in the elderly is similar to that in other age groups, but may require a gentler approach due to patients’ frailty. Rehabilitation is also important to help the elderly regain function and prevent long-term complications.
TIA symptoms: a warning sign of stroke
A transient ischemic attack (TIA) is a warning sign of stroke. It occurs when blood flow to a part of the brain is temporarily interrupted, causing symptoms similar to those of a full-blown stroke.
Symptoms of TIA can include weakness or paralysis on one side of the body, difficulty speaking or understanding language, vision problems and dizziness. These symptoms may last from a few minutes to a few hours, but should not be ignored.
The aim of TIA treatment is to prevent a full-blown stroke. This may include medication to reduce the risk of blood clots, lifestyle changes such as quitting smoking and modifying diet, and management of risk factors such as high blood pressure and diabetes.
Stroke rehabilitation: what does it involve?
Stroke rehabilitation is a complex, multifaceted process that plays a crucial role in the patient’s recovery. It generally begins as soon as the patient’s condition stabilizes, often in the first few days following the stroke. The main aim of rehabilitation is to maximize the patient’s recovery, helping them to regain as much of their lost functional and cognitive abilities as possible, while promoting adaptation to any residual limitations.
Specific rehabilitation goals
In addition to the general objectives already mentioned, rehabilitation after a stroke can also aim to :
- Improving muscle strength: to compensate for weaknesses resulting from stroke, particularly in the affected limbs.
- Promoting neuroplasticity: encouraging the brain to reorganize its pathways in order to recover or compensate for lost functions.
- Improve communication skills: for those with language disorders (aphasia), work on speech and comprehension.
- Reduce spasticity: manage and reduce muscle rigidity and spasms to improve mobility.
- Prevent secondary complications: such as pressure sores, deep vein thrombosis and muscle contractions.
Types of rehabilitation therapy
- Physiotherapy: Focuses on restoring motor function and mobility. It can include exercises to improve strength, balance and coordination, as well as techniques for walking again or using a wheelchair.
- Occupational therapy: helps patients regain their ability to perform everyday tasks, such as dressing, washing, cooking and working. Occupational therapy can also include home adaptations to make daily life easier.
- Speech therapy: Focusing on communication and swallowing problems, this therapy works on speech, comprehension, writing and reading, as well as on techniques for swallowing safely.
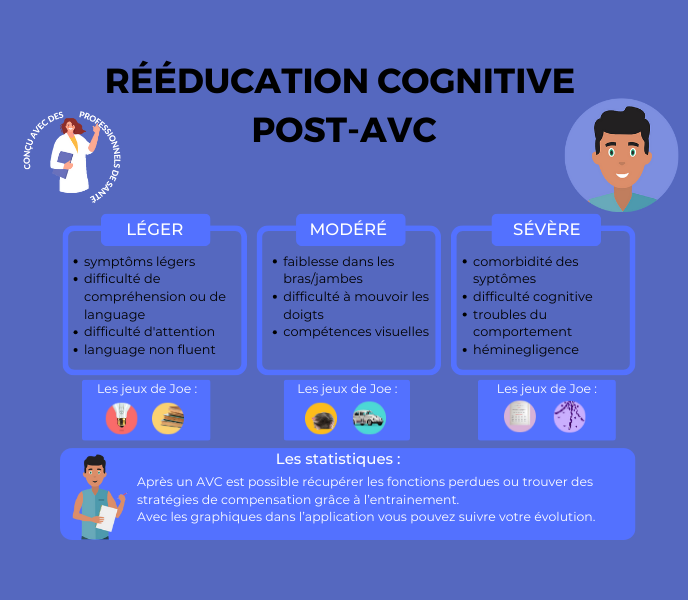
- Cognitive rehabilitation: aims to improve affected cognitive functions, such as memory, attention, problem-solving and judgment.
Multidisciplinary approach
A multidisciplinary team of doctors, nurses, physiotherapists, occupational therapists, speech therapists, neuropsychologists and social workers work together to develop a personalized rehabilitation plan. This approach addresses all aspects of the patient’s recovery, taking into account his or her medical, physical, emotional and social needs.
Importance of family support
The role of family and friends is also crucial in the rehabilitation process. Their support can greatly affect the patient’s motivation and commitment to rehabilitation. They can also be trained in certain care techniques to help patients at home.
Stroke prevention: how to reduce the risk?
Stroke prevention is essential to reduce the burden of this serious medical condition. There are several steps you can take to reduce your risk of stroke.
Preventive measures include controlling high blood pressure, maintaining a healthy weight, managing diabetes and high cholesterol, and stopping smoking. It’s also important to eat a balanced diet, rich in fruit and vegetables, and to limit consumption of foods rich in saturated fats and salt.
Lifestyle habits to reduce the risk of stroke include regular exercise, at least 30 minutes a day, five days a week, limiting alcohol consumption and reducing stress.
Here are some additional preventive measures:
- Regular medical monitoring: Regular check-ups can help detect and manage stroke risk factors at an early stage.
- Health education: Being informed about the signs and symptoms of stroke can enable early intervention, which is crucial to reducing potential damage.
- Stress management: Adopting stress management strategies can reduce certain risks associated with modifiable risk factors, such as hypertension.
Finally, there are preventive treatments available for some people at high risk of stroke, such as the use of anticoagulant drugs to prevent blood clots in people with atrial fibrillation.
Stroke is a serious medical condition that can have devastating consequences. There are two types of stroke: ischemic stroke and hemorrhagic stroke, each with its own causes, symptoms and treatments. It’s important to be aware of the risk factors common to both types of stroke, as well as those specific to certain groups, such as the young, women and the elderly. Stroke rehabilitation is essential to help patients recover their function and improve their quality of life. Finally, stroke can be prevented by adopting healthy lifestyle habits and managing risk factors.
AND FOR FURTHER INFORMATION
CLINT, YOUR BRAIN COACH
With your JOE brain coach, you choose which cognitive functions to target: attention, concentration, executive functions, mental agility, strategy implementation, … A fun and efficient program that accompanies you every day, from your smartphone or tablet!

REMOTE MEMORY COACHING
Other articles that might interest you:
No Results Found
The page you requested could not be found. Try refining your search, or use the navigation above to locate the post.