Stroke recurrence, the reappearance of stroke symptoms after an initial episode, poses a significant threat to individuals who have already experienced this neurological event. Defined as the sudden interruption of blood flow to the brain, strokes often leave lasting consequences, affecting mobility, cognition, and overall quality of life. The impact of stroke recurrence reverberates not only through the individual’s health but also through their families and communities, highlighting the urgency of effective prevention strategies.
In the realm of healthcare, preventing stroke recurrence stands as a paramount objective. The recurrence of stroke not only compounds existing disabilities but also elevates the risk of further complications, including mortality. Consequently, there is a pressing need to implement comprehensive preventive measures aimed at minimizing the likelihood of subsequent strokes. Recognizing the significance of proactive intervention, individuals, healthcare providers, and policymakers alike must prioritize education, lifestyle modifications, and appropriate medical interventions to mitigate the risk of stroke recurrence and enhance the well-being of those affected by this debilitating condition.
Understanding Stroke Risk Factors
Understanding stroke risk factors is akin to assembling a puzzle where each piece represents a different element that could potentially contribute to this complex medical condition. Recognizing these pieces is crucial because it gives us the power to see the bigger picture and, more importantly, to take action to prevent strokes from happening in the first place. Let’s delve deeper into these risk factors and explore how we can address them in a supportive and proactive manner.
Hypertension, Diabetes, and High Cholesterol: These three conditions are among the most significant risk factors for stroke. Imagine them as warning signs on the road to health, signaling the need for immediate attention and action. Managing these conditions with the help of healthcare professionals through medication, diet, and lifestyle changes can significantly reduce the risk of stroke. It’s like adjusting your speed and direction after seeing a warning sign, keeping you safely on the path to well-being.
Lifestyle Factors: Smoking, excessive alcohol consumption, and physical inactivity are not just bad habits; they are detours that lead away from health. Each puff of smoke, excessive drink, or day spent sedentary increases the risk of stroke. The good news is that these are factors we can control. Quitting smoking, moderating alcohol intake, and incorporating physical activity into our daily routines are steps we can take to get back on the main road to health. Think of these changes not as sacrifices, but as investments in a healthier, more vibrant future.
Cardiovascular Diseases and Atrial Fibrillation: These conditions are like roadblocks in our journey to health, making it harder for the blood to flow smoothly and increasing the risk of stroke. Working closely with healthcare professionals to manage these conditions can help clear the path and reduce the risk. This may involve medication, lifestyle changes, or even surgical interventions, but the goal is always to keep moving forward toward better health.
Obesity: Carrying excess weight is like carrying a heavy burden on this journey, making every step harder and increasing the risk of stroke. Addressing obesity through a combination of diet, exercise, and sometimes medical intervention can lighten the load significantly. It’s about making the journey easier and reducing the risk of numerous health conditions, including stroke.
Taking Action: Understanding these risk factors empowers us to take control of our health. By adopting preventive measures such as maintaining a healthy diet, exercising regularly, and monitoring our health conditions, we can significantly reduce our stroke risk. It’s about making informed choices every day that lead to a healthier life.
Healthcare Professionals’ Role: Healthcare providers play a crucial role in this journey. They are the guides that can help navigate the complex landscape of stroke prevention, offering advice, treatment, and support tailored to each individual’s needs. Through effective management of underlying health conditions and collaboration with patients on lifestyle modifications, healthcare professionals can help reduce the incidence of stroke and its impact on individuals and communities.
Understanding stroke risk factors is the first step on a path to prevention. It’s about recognizing the risks, making changes, and seeking support when needed. With the right knowledge and actions, we can all contribute to reducing the burden of stroke and leading healthier, more fulfilling lives.
Medical Interventions for Stroke Prevention
Medical interventions for stroke prevention encompass a spectrum of approaches aimed at mitigating the risk of stroke occurrence and recurrence. Medication management plays a central role in this endeavor, with anticoagulants, antiplatelet agents, and statins often prescribed to regulate blood clotting, reduce plaque buildup, and manage cholesterol levels, respectively.
For high-risk patients, surgical options offer additional avenues for stroke prevention. Procedures such as carotid endarterectomy and angioplasty with stenting help alleviate arterial blockages and restore optimal blood flow to the brain, thus minimizing the likelihood of ischemic stroke. By integrating medication management and surgical interventions tailored to individual patient profiles, healthcare providers can effectively mitigate the risk of stroke and enhance overall patient outcomes, underscoring the importance of a comprehensive approach to stroke prevention within clinical practice.
Lifestyle Modifications for Stroke Prevention
Lifestyle modifications serve as cornerstone strategies for stroke prevention, encompassing dietary changes, and physical activity regimens. Dietary alterations involve adopting a heart-healthy approach, emphasizing the consumption of fruits, vegetables, whole grains, and lean proteins while limiting sodium, saturated fats, and processed foods. Such nutritional choices help maintain optimal blood pressure and cholesterol levels, key determinants in stroke risk reduction.
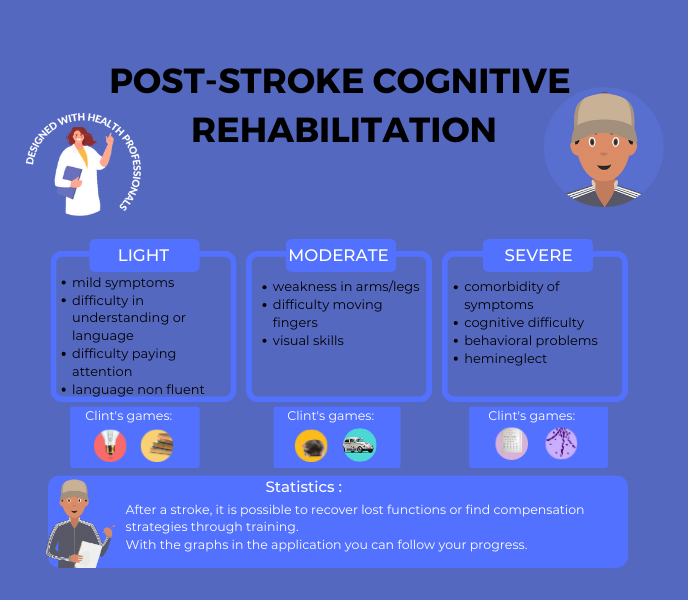
Concurrently, engaging in regular physical activity and adhering to exercise regimens contribute to overall cardiovascular health and weight management. Activities such as brisk walking, swimming, or cycling not only enhance blood circulation and strengthen the heart but also lower the likelihood of obesity and diabetes, major contributors to stroke incidence. By embracing these lifestyle modifications, individuals can proactively mitigate their risk of stroke and promote long-term health and well-being, while doing brain traning programs.
Stress Management Techniques
Stress management techniques encompass various approaches aimed at mitigating the detrimental effects of stress on physical and mental well-being. Mindfulness and meditation practices, including deep breathing exercises and guided meditation sessions, promote relaxation and cultivate present-moment awareness, thereby reducing stress levels and fostering emotional resilience.
Additionally, stress reduction strategies encompass a range of techniques such as time management, prioritization, and setting boundaries to alleviate overwhelming feelings and promote a sense of control. Engaging in hobbies, social support networks, and seeking professional counseling are also integral components of stress reduction strategies. By incorporating mindfulness practices and stress reduction techniques into daily routines, individuals can effectively manage stress, enhance coping mechanisms, and cultivate a greater sense of balance and inner peace amidst life’s challenges.
Monitoring and Managing Blood Pressure
Monitoring and managing blood pressure is a critical aspect of preventive healthcare, especially for individuals at risk of stroke and cardiovascular events. Blood pressure serves as a key indicator of cardiovascular health, reflecting the force exerted by circulating blood against the walls of arteries. Regular monitoring allows healthcare providers to assess baseline levels, track fluctuations, and identify trends indicative of potential health concerns.
By implementing proactive measures such as lifestyle modifications, medication management, and adherence to treatment plans, individuals can effectively manage blood pressure levels and reduce the risk of stroke and other cardiovascular complications. Through collaborative efforts between patients and healthcare professionals, monitoring and managing blood pressure become integral components of comprehensive stroke prevention strategies.
Importance of Blood Pressure Control
The importance of blood pressure control cannot be overstated in the realm of stroke prevention and overall cardiovascular health. Elevated blood pressure, or hypertension, significantly increases the risk of stroke by placing undue strain on blood vessels, compromising their integrity, and promoting the formation of blood clots.
Moreover, uncontrolled hypertension contributes to the development of other cardiovascular conditions, including heart disease and kidney dysfunction, further exacerbating the risk of stroke recurrence. By prioritizing blood pressure control through lifestyle modifications, such as dietary changes, regular exercise, and stress management techniques, individuals can mitigate the detrimental effects of hypertension and safeguard their vascular health. Additionally, adherence to prescribed medications and regular monitoring facilitates early detection of hypertension-related complications, enabling timely intervention and improved health outcomes.
Techniques for Blood Pressure Management
Several techniques are available for effectively managing blood pressure levels and reducing the risk of stroke and other cardiovascular events. Lifestyle modifications, including adopting a balanced diet rich in fruits, vegetables, and whole grains while limiting sodium intake, play a pivotal role in blood pressure management. Regular physical activity, such as brisk walking, swimming, or cycling, helps maintain cardiovascular fitness and promotes healthy blood flow. Stress management techniques, such as mindfulness meditation, deep breathing exercises, and relaxation techniques, aid in reducing stress levels and mitigating hypertension. Additionally, medication management, under the guidance of healthcare professionals, may be necessary to achieve target blood pressure goals.
By combining these techniques and incorporating them into daily routines, individuals can effectively manage blood pressure levels and enhance their overall cardiovascular health, thus reducing the risk of stroke recurrence and promoting longevity and well-being.
Smoking Cessation Programs
Smoking cessation programs play a pivotal role in reducing the risk of stroke recurrence by addressing the significant impact of smoking on cardiovascular health. Smoking is a major modifiable risk factor for stroke recurrence, as it contributes to the narrowing and hardening of blood vessels, increases blood pressure, and promotes the formation of blood clots—all of which heighten the likelihood of stroke occurrence.
Recognizing the critical need for support systems in smoking cessation, programs offer a multifaceted approach that includes behavioral counseling, pharmacotherapy, and peer support networks. These programs aim to address nicotine dependence, identify triggers for smoking, and provide individuals with the necessary tools and resources to overcome withdrawal symptoms and maintain long-term abstinence. By actively engaging in smoking cessation programs and adopting a smoke-free lifestyle, individuals can significantly reduce their risk of stroke recurrence and improve overall cardiovascular health outcomes.
Alcohol Consumption and Stroke Risk
Alcohol consumption can have a significant impact on the risk of stroke recurrence, with both excessive and moderate drinking habits influencing vascular health. Heavy alcohol consumption is associated with an increased risk of stroke recurrence, as it raises blood pressure, disrupts normal heart rhythm, and contributes to the development of atrial fibrillation and other cardiovascular conditions.
Conversely, moderate alcohol consumption, defined as up to one drink per day for women and up to two drinks per day for men, may have a protective effect against ischemic stroke, primarily through its influence on cholesterol levels and blood clotting. Guidelines for responsible drinking emphasize moderation, encouraging individuals to be mindful of their alcohol intake, stay within recommended limits, and consider personal health factors when making alcohol-related decisions. By adhering to responsible drinking guidelines, individuals can minimize their risk of stroke recurrence and promote overall cardiovascular health.
Sleep Hygiene and Stroke Prevention
Sleep hygiene plays a crucial role in stroke prevention, as the quality and duration of sleep have a profound impact on cardiovascular health. The link between sleep disorders, such as obstructive sleep apnea (OSA) and insomnia, and stroke risk is well-established. OSA, characterized by interrupted breathing during sleep, can lead to hypertension, atrial fibrillation, and other cardiovascular complications that increase the likelihood of stroke.
Similarly, chronic insomnia is associated with higher levels of inflammation and sympathetic nervous system activity, further elevating stroke risk. To improve sleep quality and mitigate stroke risk, individuals can adopt various tips, including maintaining a consistent sleep schedule, creating a relaxing bedtime routine, optimizing sleep environment, avoiding stimulants before bedtime, and seeking treatment for underlying sleep disorders. By prioritizing good sleep hygiene practices, individuals can enhance overall cardiovascular health and reduce the risk of stroke recurrence.
Regular Health Checkups and Screenings
Regular health checkups and screenings play a crucial role in maintaining optimal health and preventing serious medical conditions, including stroke. Routine health assessments, encompassing physical examinations, blood tests, and screenings for conditions such as hypertension, diabetes, and high cholesterol, provide valuable insights into one’s overall well-being and identify potential risk factors for stroke.
The importance of early detection cannot be overstated, as many underlying health conditions associated with stroke, such as atrial fibrillation and carotid artery disease, may not present noticeable symptoms in their early stages. Through early detection and intervention, healthcare providers can implement timely treatment plans, lifestyle modifications, and preventive measures to mitigate the risk of stroke and other cardiovascular events. Thus, regular health checkups serve as proactive measures in promoting early detection, enabling timely intervention, and ultimately safeguarding individuals against the devastating consequences of stroke.
Family and Community Support Systems
Family and community support systems are instrumental in stroke prevention efforts, offering valuable resources and networks to promote health and well-being. Engaging family members in stroke prevention involves raising awareness about risk factors, encouraging healthy lifestyle choices, and fostering open communication about individual health concerns. Families can provide emotional support, encouragement, and accountability for adopting and maintaining healthy behaviors such as regular exercise, nutritious eating, and medication adherence. Additionally, utilizing community resources and programs expands access to educational materials, support groups, and preventive services tailored to stroke prevention.
Community-based initiatives may include wellness workshops, fitness classes, and screenings for early detection of cardiovascular risk factors. By leveraging family support and community resources, individuals can enhance their resilience against stroke and cultivate a supportive environment conducive to long-term health and wellness.
Empowering stroke survivors for recurrence prevention is paramount to enhancing their quality of life and reducing the risk of subsequent debilitating events. Through comprehensive strategies encompassing medical interventions, lifestyle modifications, and support systems, individuals can actively mitigate the likelihood of stroke recurrence. By addressing modifiable risk factors such as hypertension, smoking, and sedentary lifestyles, survivors can take proactive steps towards optimizing their cardiovascular health and minimizing the risk of future strokes.
Furthermore, fostering partnerships with healthcare providers, families, and communities ensures access to resources, support networks, and educational opportunities tailored to stroke prevention. Ultimately, by empowering stroke survivors with knowledge, tools, and support, we can collectively work towards a future where the burden of stroke recurrence is significantly reduced, and survivors can thrive with confidence in their long-term health and well-being.
AND FOR FURTHER INFORMATION

CLINT, YOUR BRAIN COACH
With your JOE brain coach, you choose which cognitive functions to target: attention, concentration, executive functions, mental agility, strategy implementation, etc. A fun, efficient program that supports you every day.
Other articles that might interest you:
Reconstructing After Stroke: Redefining Identity and Goals.
A stroke is a serious medical condition that occurs when blood flow to the brain is interrupted, causing damage to...
The Different Types of Stroke Explained: Ischemic, Hemorrhagic and TIA.
A stroke is a serious medical condition that occurs when blood flow to a part of the brain is interrupted or reduced,...
Preventing Stroke Recurrence: Measures and Lifestyle Changes.
A stroke is a serious medical condition that occurs when blood flow to the brain is interrupted, causing damage to...