The immediate aftermath of a stroke marks a critical juncture in the journey toward recovery, presenting both challenges and opportunities for patients and their families. Recognizing the significance of the first steps following a stroke is paramount, as they can profoundly impact the individual’s long-term prognosis and quality of life. In these pivotal moments, swift and informed actions can mitigate the severity of potential impairments and facilitate the restoration of function.
Navigating the complexities of stroke recovery requires a comprehensive understanding of the physiological, emotional, and logistical aspects involved. From accessing timely medical intervention to establishing a supportive care network, each decision carries weight in shaping the trajectory of recovery. Moreover, the role of family members and caregivers in this process cannot be overstated, as their unwavering support can instill hope and motivation in the face of adversity.
In this guide, we explore the critical importance of the initial steps taken after a stroke, offering insights and strategies to empower patients and their families on the path to recovery.
Understanding Stroke and its Effects
A stroke occurs when there is a disruption in the blood supply to the brain, resulting in the sudden loss of brain function. This disruption can be caused by either a blockage in an artery (ischemic stroke) or the rupture of a blood vessel (hemorrhagic stroke). Regardless of the type, the consequences of a stroke can be profound and varied.
Common physical effects include paralysis or weakness on one side of the body, difficulty with balance and coordination, and challenges with speech and swallowing. Additionally, strokes can lead to cognitive impairments such as memory loss, difficulty with problem-solving and decision-making, and changes in behavior and emotions. Understanding these potential effects is crucial for both patients and caregivers to navigate the complexities of stroke recovery and rehabilitation effectively.
Immediate Actions After a Stroke
Seeking emergency medical assistance is paramount upon recognizing the signs and symptoms of a stroke, including sudden numbness, weakness, difficulty speaking, or a severe headache. Time sensitivity is crucial as immediate intervention significantly enhances prognosis. Emergency services provide rapid access to specialized care and diagnostic procedures tailored to stroke patients. Following arrival at the medical facility, patients undergo a comprehensive initial assessment encompassing physical examination, neurological evaluation, and imaging studies like CT scans or MRI scans to determine stroke type and severity.
Medical professionals promptly initiate appropriate treatment measures, such as clot-busting medications for ischemic strokes or interventions to control bleeding in hemorrhagic strokes. Supportive therapies like oxygen supplementation and blood pressure management aim to stabilize patients and optimize recovery outcomes, emphasizing the critical importance of swift medical attention in managing acute stroke events.
Transitioning to Rehabilitation
As individuals progress beyond the acute phase of a stroke, a pivotal step involves transferring to a dedicated stroke unit or rehabilitation facility. This move ensures specialized care tailored to the unique needs of stroke survivors. The rehabilitation journey commences with an introduction to the multidisciplinary rehabilitation team, comprising physiatrists, physical therapists, occupational therapists, speech therapists, and other specialists. This collaborative team works closely with patients to formulate personalized rehabilitation plans addressing physical, cognitive, and emotional aspects.
The rehabilitation process focuses on restoring functionality, enhancing independence, and adapting to the challenges posed by the stroke. Through a combination of targeted exercises, therapeutic interventions, and ongoing support, patients embark on a path towards regaining optimal quality of life and maximizing their recovery potential.
Physical Rehabilitation
Physical rehabilitation after a stroke encompasses a range of interventions aimed at restoring mobility, strength, and overall physical function. Physical therapy exercises focus on improving muscle tone, coordination, and balance through targeted movements and activities tailored to the individual’s abilities and goals. These exercises may include gait training, range of motion exercises, and strength-building activities designed to enhance motor control and promote independence in daily activities.
Concurrently, occupational therapy plays a crucial role in facilitating the transition back to daily living activities. Occupational therapists work with stroke survivors to address challenges related to self-care, household tasks, and work-related activities by incorporating adaptive strategies, assistive devices, and environmental modifications to promote safety and efficiency. Together, physical and occupational therapies form integral components of stroke rehabilitation, empowering individuals to regain autonomy and engage meaningfully in their daily lives.
Cognitive and Speech Therapy
Cognitive and speech therapy are essential components of rehabilitation following a stroke, addressing the diverse challenges survivors face in communication and cognitive function. Speech therapists employ various techniques to address speech and language difficulties, including articulation exercises, language comprehension tasks, and strategies to improve verbal expression and fluency. Additionally, they may incorporate alternative communication methods such as augmentative and alternative communication (AAC) devices to facilitate effective communication. Concurrently, cognitive therapy targets deficits in memory, attention, and problem-solving skills, helping individuals regain cognitive function and independence in daily activities.
Through personalized interventions and targeted exercises, cognitive therapists work collaboratively with patients to enhance cognitive abilities, promote mental flexibility, and improve overall cognitive functioning, fostering meaningful recovery and participation in everyday life.
Emotional Support for Patients and Families
Emotional support for patients and families is vital in navigating the profound impact of stroke on mental well-being and interpersonal dynamics. Coping with emotional changes after a stroke requires acknowledgment of the complex array of feelings, including grief, frustration, anxiety, and depression, that may arise in both patients and their loved ones. Open communication and validation of emotions within the family unit create a supportive environment for processing and adapting to life post-stroke.
Furthermore, accessing support groups and counseling services offers valuable opportunities for individuals to connect with others facing similar challenges, share experiences, and learn coping strategies. Professional counseling provides a safe space for exploring emotions, developing resilience, and acquiring practical tools to manage stressors effectively. By prioritizing emotional well-being and fostering a supportive network, patients and families can navigate the emotional journey of stroke recovery with greater resilience and mutual understanding.
Nutritional Support and Lifestyle Changes
Nutritional support and lifestyle changes play integral roles in stroke recovery and prevention. Dietary adjustments for stroke recovery involve adopting a heart-healthy eating plan rich in fruits, vegetables, whole grains, lean proteins, and healthy fats while limiting sodium, saturated fats, and added sugars. These dietary modifications can help manage risk factors such as high blood pressure, cholesterol levels, and blood sugar levels, thereby promoting cardiovascular health and facilitating recovery.
Additionally, promoting healthy lifestyle habits for the prevention of future strokes involves engaging in regular physical activity, maintaining a healthy weight, managing stress levels, and avoiding tobacco and excessive alcohol consumption. By embracing these lifestyle changes, individuals can reduce their risk of recurrent strokes and enhance their overall well-being, fostering long-term health and vitality.
Home Modifications and Assistive Devices
Home modifications and assistive devices stand as the silent heroes in the journey of stroke recovery, transforming ordinary living spaces into sanctuaries of safety, independence, and empowerment. This transformation goes beyond mere physical adjustments; it’s about rekindling the sense of belonging and capability within one’s own space, enabling stroke survivors to navigate their world with dignity and resilience.
Creating a Safe Haven: The process of adapting a home for safety and accessibility is akin to tailor-making a suit—it’s about ensuring a perfect fit for the individual’s needs and challenges. This might mean reimagining the layout to eliminate hazards like slippery floors and uneven surfaces that pose risks of falls. Simple yet effective modifications, such as securing rugs, can make a significant difference in preventing accidents. Similarly, addressing architectural barriers like narrow doorways can make the home more wheelchair-friendly, ensuring smooth passage from room to room.
Empowerment through Adaptation: Installing grab bars in strategic locations such as bathrooms and along hallways offers not just support, but a newfound confidence in moving around. Ramps and stairlifts open up the home, making every corner accessible and eliminating the daunting obstacle that stairs often represent post-stroke. These adaptations are not just about mobility; they’re about reclaiming independence and the freedom to move within one’s own space without fear.
Assistive Devices: Tools of Independence: The role of assistive devices in stroke recovery cannot be overstated. Mobility aids like walkers and wheelchairs become extensions of the individual, offering the support needed to explore and engage with the world. Reachers and dressing aids transform what were once frustrating tasks into manageable activities, restoring a sense of self-sufficiency. Adaptive utensils and specially designed kitchen tools empower survivors to enjoy meals and participate in cooking, an activity that is not only essential but also deeply connected to family and cultural traditions.
A Personal Touch: Beyond the practicality of these modifications and devices lies a deeper significance—the personalization of space to fit the unique journey of each stroke survivor. This personal touch can include adaptive furniture that provides comfort and support, or the arrangement of living spaces in a way that promotes ease of movement and accessibility. Every adjustment, no matter how small, is a step towards creating a living environment that reflects the individual’s needs, tastes, and lifestyle.
The Psychological Impact: Beyond the physical benefits, the psychological uplift that comes from being able to navigate and perform tasks in one’s own home is profound. This sense of autonomy and normalcy can significantly impact a survivor’s mental health, enhancing their well-being and motivation during the recovery process. The home, once a place of potential hazards, becomes a sanctuary of healing and independence, a space where survivors can feel secure, capable, and above all, at home.
In essence, home modifications and assistive devices are more than just practical solutions; they are vital elements in the tapestry of stroke recovery, woven with the threads of safety, independence, and personal empowerment. They play a pivotal role in transforming the home from a place of challenges to a space of possibilities, enabling stroke survivors to live fully and confidently within their sanctuaries of recovery and renewal.
Follow-up Care and Long-Term Recovery
Follow-up care and long-term recovery are essential aspects of stroke management, ensuring ongoing support and optimization of rehabilitation outcomes. Regular medical check-ups and monitoring enable healthcare professionals to assess the individual’s progress, monitor for potential complications, and adjust treatment plans as needed. These check-ups often include evaluations of blood pressure, cholesterol levels, and medication management to mitigate the risk of recurrent strokes and manage underlying health conditions. Moreover, adjusting rehabilitation goals for long-term recovery involves revisiting and adapting therapy plans to address evolving needs, challenges, and aspirations.
This process may entail setting new milestones, incorporating advanced therapeutic techniques, and fostering continued engagement in rehabilitation activities to promote sustained progress and quality of life for stroke survivors as they navigate their journey toward recovery.
Educating Patients and Families About Stroke Prevention
Understanding risk factors for stroke recurrence
Understanding the risk factors for stroke recurrence is essential for patients and their families to effectively manage their health post-stroke. Common risk factors include hypertension, diabetes, high cholesterol levels, smoking, obesity, and a sedentary lifestyle. By recognizing these risk factors, individuals can work with healthcare professionals to develop personalized prevention strategies aimed at reducing the likelihood of experiencing another stroke.
Moreover, understanding the interplay between these risk factors and their impact on vascular health empowers patients and families to make informed decisions regarding lifestyle choices and medical management. Education about risk factors serves as a cornerstone in stroke prevention efforts, enabling individuals to take proactive steps to protect their health and minimize the risk of recurrent strokes.
Implementing preventive measures and lifestyle changes
AND FOR FURTHER INFORMATION

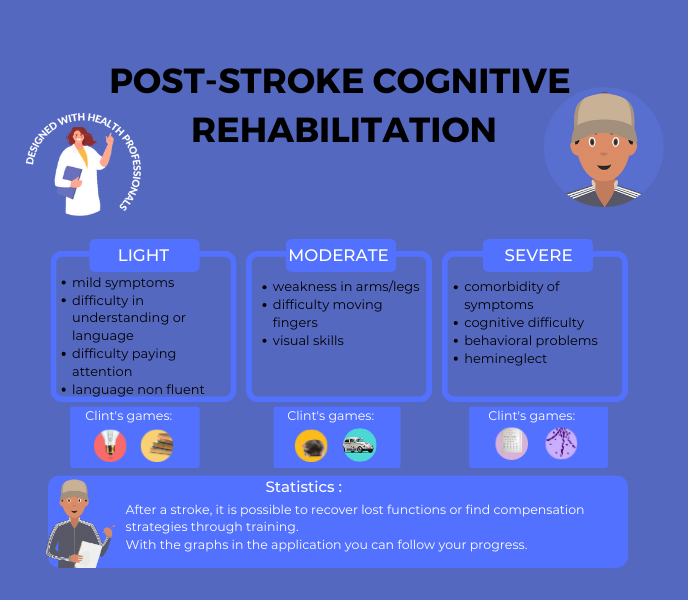
CLINT, YOUR BRAIN COACH
With your JOE brain coach, you choose which cognitive functions to target: attention, concentration, executive functions, mental agility, strategy implementation, etc. A fun, efficient program that supports you every day.
Other articles that might interest you:
Reconstructing After Stroke: Redefining Identity and Goals.
A stroke is a serious medical condition that occurs when blood flow to the brain is interrupted, causing damage to...
The Different Types of Stroke Explained: Ischemic, Hemorrhagic and TIA.
A stroke is a serious medical condition that occurs when blood flow to a part of the brain is interrupted or reduced,...
Preventing Stroke Recurrence: Measures and Lifestyle Changes.
A stroke is a serious medical condition that occurs when blood flow to the brain is interrupted, causing damage to...