Introduction: A Paradigm Shift in Progress
Long considered as symptoms to “treat” with medication, behavioral disorders associated with neurodegenerative diseases are now the subject of a radically different approach. National and international recommendations are unanimous: non-pharmacological approaches must constitute the first line of intervention, with the use of psychotropic drugs only being considered in case of failure or insufficiency of these approaches, and for the most severe situations.
This paradigm shift is not just a theoretical evolution. It is based on increasingly solid scientific evidence demonstrating both the effectiveness of many non-pharmacological interventions and the limitations, even dangers, of systematic medication-based approaches in frail elderly people.
At the beginning of 2025, where do we stand? What are the validated approaches, those that are emerging, those that still require research? This article offers a complete and updated overview of non-pharmacological approaches to behavioral disorders, to guide professionals and families in their care choices.
—
Why Favor Non-Pharmacological Approaches?
The Limitations of Drug Treatments
Psychotropic medications used in behavioral disorders of elderly people have significant limitations.
Modest effectiveness: Clinical studies show that the effectiveness of antipsychotics on behavioral symptoms of dementia is statistically significant but clinically modest. The difference between the medication and placebo is often small.
Significant side effects: Excessive sedation, falls, parkinsonian syndrome, swallowing disorders, cerebrovascular accidents, increased mortality… The list of adverse effects is long and concerning in this vulnerable population.
An unfavorable benefit/risk ratio: In 2025, health agencies maintain their alerts on the use of antipsychotics in elderly people with dementia, due to an increased mortality risk of 60% to 70%.
The absence of fundamental treatment: Medications do not address the causes of behavioral disorders but only their manifestations. They do not provide a lasting solution.
The Strengths of Non-Pharmacological Approaches
Conversely, non-pharmacological approaches have considerable advantages.
A person-centered approach: Rather than suppressing a symptom, they seek to understand the causes of the behavior and respond to them appropriately.
The absence of major side effects: When properly conducted, these approaches do not present significant health risks.
Often lasting effects: By modifying the environment, care practices, or modes of communication, we act on the factors that maintain the disorders.
A global improvement in quality of life: Beyond reducing behavioral disorders, these approaches often contribute to the person’s overall well-being.
A benefit for the entourage: Care teams and families trained in these approaches report an improvement in their own professional or personal quality of life.
—
Relational Approaches: The Heart of the System
Validation According to Naomi Feil
Developed in the 1980s, Naomi Feil’s Validation method remains a major reference in 2025. It proposes to enter the emotional world of the disoriented person rather than confronting them with a reality they can no longer integrate.
Key principles include unconditional acceptance of the person’s experience, validation of emotions rather than facts, use of specific techniques (reformulation, open questions, touch, eye contact), and respect for the person’s stage of disorientation.
Studies show Validation’s effectiveness on agitation, anxiety, and disruptive behaviors, as well as an improvement in the emotional well-being of accompanied individuals.
The Humanitude Approach
Developed in France by Yves Gineste and Rosette Marescotti, Humanitude is a care philosophy that places relationships at the heart of support. It is based on four pillars: gaze, speech, touch, and verticality.
In 2025, Humanitude has spread widely in French and international facilities. Studies show a significant reduction in agitation and resistance to care behaviors, a decrease in the use of restraints and psychotropic drugs, as well as an improvement in care team satisfaction.
The Adapted Montessori Approach
Initially designed for children’s education, the Montessori method was adapted for elderly people with cognitive disorders by Dr. Cameron Camp. It offers meaningful activities that build on preserved abilities.
Fundamental principles are respect for the person’s pace and choices, offering activities with meaning and purpose, adapting tasks to remaining abilities, and an environment prepared to promote autonomy.
This approach is particularly effective against apathy and can reduce disruptive behaviors by providing a sense of usefulness and control.
—
Sensory Approaches: Stimulating to Soothe
Music Therapy
Music therapy is one of the best-studied and most effective non-pharmacological approaches for behavioral disorders related to dementia.
Recent meta-analyses confirm a significant effect on agitation, anxiety, depressive symptoms, as well as an improvement in social interactions and quality of life. Personalized music (based on the person’s preferences) seems more effective than generic music.
Validated protocols include individualized music listening, active music therapy (singing, percussion), and group sessions led by a music therapist.
Aromatherapy
The use of essential oils in supporting behavioral disorders is developing, with growing evidence of effectiveness.
The most studied oils are true lavender (Lavandula angustifolia) for its relaxing properties, lemon balm (Melissa officinalis) for agitation and anxiety, and rosemary for cognitive stimulation.
Studies show modest but significant effects on agitation, with the advantage of good tolerance. Precautions for use (dilution, modes of administration) must be respected.
Light Therapy
Light plays a central role in regulating circadian rhythms, often disrupted in dementia. Light therapy involves exposing the person to bright light (2500 to 10000 lux) for 30 minutes to 2 hours, usually in the morning.
Studies show effectiveness on sleep disorders, nocturnal agitation, sundowning syndrome, and potentially on depressive symptoms.
In 2025, “dynamic light” systems are developing in institutions, reproducing natural light variations throughout the day.
The Snoezelen Approach
Snoezelen spaces (contraction of “snuffelen”: to sniff, and “doezelen”: to doze in Dutch) offer controlled multisensory stimulation in a soothing environment.
Typical elements include bubble tubes, luminous optical fibers, image projectors, aroma diffusers, varied tactile surfaces, and soft music.
Studies show a reduction in agitation and disruptive behaviors during and after sessions, as well as an improvement in emotional well-being. The effect, however, seems temporary and requires regular sessions.
—
Environmental Approaches: The Environment as Care
The Therapeutic Garden
Access to a natural outdoor space has multiple benefits for people with behavioral disorders.
Documented effects include a reduction in agitation and disruptive behaviors, improved sleep, decreased stress (lower cortisol), and a sense of freedom and well-being.
Characteristics of an effective therapeutic garden include a secure wandering circuit without dead ends, varied spaces (shade/sun, benches, pergolas), sensory elements (fragrant plants, fountain), and possible activities (adapted gardening).
Architectural Design
Architecture and the design of living spaces significantly influence behaviors.
Principles recommended in 2025 are creating human-scale spaces (small units), clear and adapted signage, optimized natural lighting, soothing and contrasting colors for landmarks, reduction of excessive stimulation (noise, agitation), and personalization of individual spaces.
Reduction of Restraints
The policy of reducing restraints (physical and chemical) is an integral part of non-pharmacological approaches. It requires reflection on the environment, care practices, and possible alternatives.
Facilities engaged in this approach generally report a paradoxical decrease in falls and behavioral disorders, contrary to initial fears.
—
Activity-Based Approaches: Giving Meaning
Therapeutic Reminiscence
Reminiscence therapy uses memories from the past to improve present well-being. It relies on the relative preservation of old memory in dementia.
Supports used include family photos and albums, objects from the past, period music, old videos and films, and discussions about life history.
Studies show positive effects on mood, social interactions, and potentially on certain behavioral disorders. The approach requires knowledge of the person’s life history.
Art Therapy
Art therapy offers artistic creation activities (painting, drawing, modeling, collage) supervised by a trained professional.
Observed benefits are emotional expression through a non-verbal channel, valorization and sense of accomplishment, reduction of anxiety and agitation, as well as maintenance of fine motor skills.
Adapted Physical Activities
Physical activity has multiple benefits for people with cognitive disorders: maintenance of functional autonomy, improved sleep, reduction of agitation, possible neuroprotective effect.
Adapted activities include accompanied walking, gentle gymnastics, adapted tai-chi, seated dancing, and motor courses.
—
Approaches Involving Living Beings
Animal-Assisted Therapy
The presence of animals with elderly people in institutions shows beneficial effects on well-being and behaviors.
Modalities include resident animals (cats, birds, fish), regular visits by trained dogs, and mobile educational farms.
Studies show a reduction in agitation, improved social interactions, and decreased depressive symptoms. Hygiene precautions and respect for preferences (some people don’t like animals) are essential.
The Presence of Social Robots
A novelty of recent years: social robots like PARO (seal-robot) or companion robots show effectiveness comparable to live animals on certain parameters, with practical advantages (no allergies, no care required).
Recent studies confirm an effect on agitation and apathy, as well as improved social interactions. The ethical debate on their use remains open.
—
Body-Based Approaches
Touch-Massage
Relational touch and massage adapted to elderly people can have a significant soothing effect.
Techniques used are hand massage, facial massage, foot relaxation-touch, and soothing effleurage.
Studies show a reduction in agitation, improvement in caregiver-patient relationship, and possible pain reduction. Professional training is essential.
Structured Physical Activity
Beyond occasional activities, structured exercise programs show benefits on behavioral disorders.
Validated programs include balance and strength exercises, adapted endurance activities, and combined programs (motor + cognitive).
—
Cognitive Stimulation: Maintaining Abilities
Cognitive Stimulation Programs
Regular cognitive stimulation contributes to maintaining preserved functions and can have an indirect effect on behavioral disorders by reducing frustration and apathy.
DYNSEO has developed programs specifically designed for people with cognitive disorders.
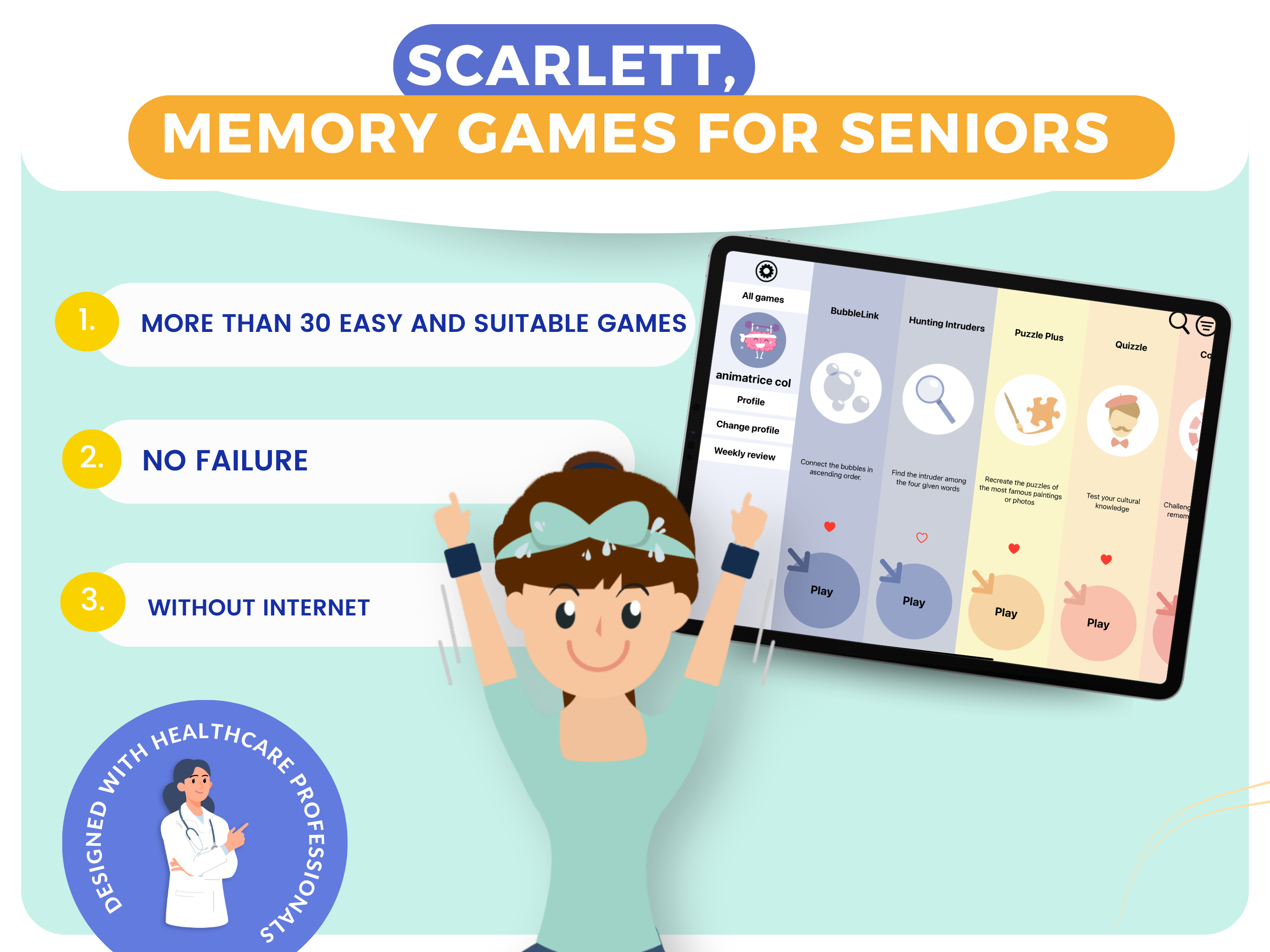
The SCARLETT program offers memory games and cognitive training adapted to seniors with diseases like Alzheimer’s’s or Parkinson’s. Activities are designed to be successful, avoiding failure situations that are sources of frustration.
The CLINT program is aimed at adults and offers varied cognitive exercises to maintain brain functions and contribute to mental well-being.
—
Implementation: Conditions for Success
Professional Training
The success of non-pharmacological approaches largely depends on team training. Understanding the mechanisms of behavioral disorders, mastering intervention techniques, knowing how to observe and analyze situations: all skills that are acquired.
DYNSEO offers comprehensive training on disease-related behavioral disorders, covering different non-pharmacological approaches and their practical implementation.

Access professional training
Family Support
Families are essential partners in care. Informing them about non-pharmacological approaches, training them in adapted communication techniques, involving them in the care plan contributes to the consistency and effectiveness of care.
DYNSEO offers specific training for families confronted with behavioral changes in their loved ones.

Access family training
Personalized Approach
There is no universal approach effective for everyone. The choice of interventions must be personalized based on the person’s preferences and life history, the type of behavioral disorder presented, the stage of the disease, available resources, and continuous evaluation of effects.
Continuous Evaluation
Non-pharmacological interventions must be evaluated regularly to measure their effectiveness and adjust them if necessary. Simple tools (agitation scales, structured observation) allow this monitoring.
—
Prospects for 2025 and Beyond
New Technologies
Virtual reality is beginning to be explored for its soothing effects (immersion in natural environments) and its ability to stimulate memories.
Artificial intelligence could allow increased personalization of interventions by analyzing behavioral data.
Connected objects facilitate behavior monitoring and real-time adaptation of interventions.
Evolution of Recommendations
Official recommendations (HAS, learned societies) continue to evolve toward an increasingly central place for non-pharmacological approaches, with growing requirements for professional training.
Remaining Challenges
Despite progress, challenges persist: funding for training and interventions, lack of time for care teams, difficulty in generalizing approaches beyond pioneering facilities, and the need for additional research for certain approaches.
—
Conclusion: A New Art of Care
The 2025 state of affairs on non-pharmacological approaches to behavioral disorders reveals a field in full maturation. Many approaches have proven their effectiveness and are now recommended as first-line treatment.
What is emerging is a new art of care, focused on the person and not on the symptom, which mobilizes the creativity and humanity of caregivers as much as their technical skills.
Training professionals, supporting families, developing adapted environments, offering meaningful activities: these are all levers that, combined, can significantly improve the quality of life of people with behavioral disorders and their entourage.
DYNSEO Resources:
—
This article was written by the DYNSEO team, specialists in cognitive support and training on behavioral disorders.